As prosperous as America is, food insecurity continues to be a wide-spread, problem around the nation. About 8.6 million adults lived in households with very low food insecurity in 2022. Some of the most vulnerable populations — children and adults — as well as people of color experience food insecurity at much higher rates.
Why are so many Americans going hungry? Food insecurity is often rooted in social determinants of health (SDOH) including race, ethnicity, income, employment status and ZIP code.
While federal programs work to address SDOH and provide critical nutrition assistance to millions of Americans, innovation around solving food insecurity is happening at the state level. A new Mom’s Meals® white paper Innovating to Overcome Food Insecurity: How states are taking new approaches to achieve better outcomes surveys the landscape of solutions and focuses on new, state-level programs that are moving the needle on food insecurity in communities around the country.
COVID-19: a catalyst for change
Food insecurity was already a serious concern when, in 2020, the COVID-19 pandemic further increased the number of Americans needing support. The global health crisis spurred rapid changes at the federal and state levels which protected millions of Americans with nutritional support and health care coverage during the pandemic. Even though the public health emergency is over, many states are continuing — and even expanding — programs that started during the pandemic.
Building on a foundation of federal programs
Long-standing federal programs, mainly Medicaid and Medicare, are the foundation of nutritional assistance for millions of Americans. Because of their size and scope, they’re also powerful forces for change. In recent years, both programs have implemented policy and funding changes to help reduce food insecurity. Here are just a few.
- Medicaid waivers — Following federal guidelines, states can use Medicaid waivers to offer home-based services to seniors and people with disabilities. Some waivers include home-delivered meals to Medicaid members. For example, Long-Term Services and Supports (LTSS) is a type of waiver that provides various kinds of support for people with chronic conditions who can’t independently care for themselves.
- State Aging Units — The Older Americans Act (OAA) supports home and community-based services to help older Americans be as independent as possible. Under OAA Title III, states receive funding they can allocate to area agencies on aging (AAA) that offer a range of services including transportation, in-home services and home-delivered meals.
- Medicare — Medicare Advantage (MA) programs are steadily incorporating food as medicine approaches to address SDOH and can be incorporated at the state level. As MA plans add post-discharge meals benefits and offer nutrition supplements and counseling to MA members who have chronic conditions, the ability to support dual eligible populations should be considered in state programs.
States are finding ways to innovate
States are busy breaking down barriers between government programs and partners. They are improving access to services and closing gaps using community-based approaches, new collaborations, pilot programs and more. Here are just three examples:
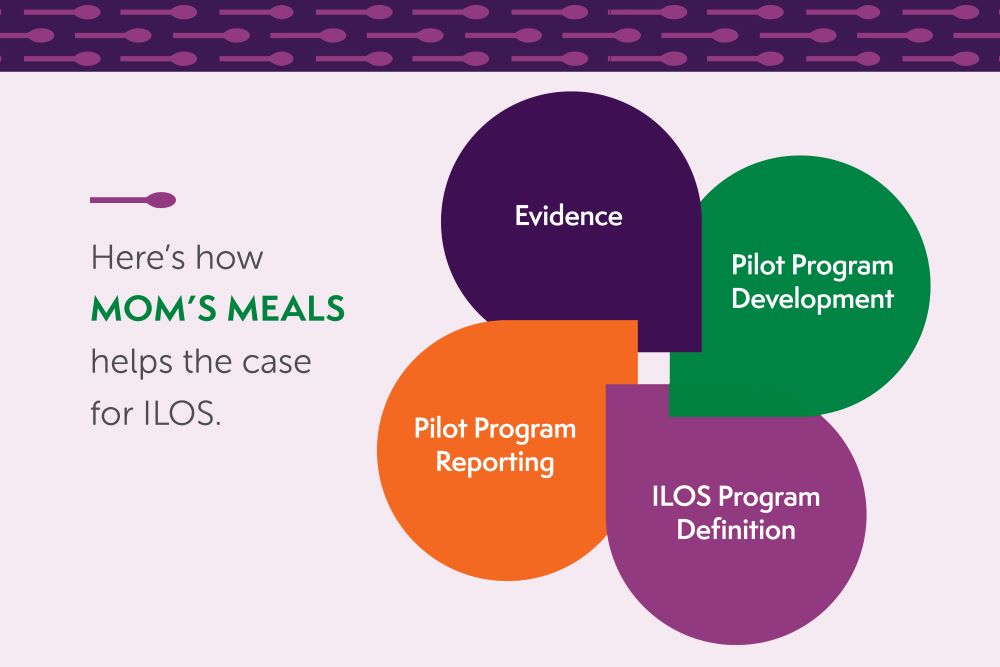
- In lieu of services (ILOS) — Under Medicaid, Centers for Medicare and Medicaid Services (CMS) offers guidance on how states and managed care plans can use ILOS to address members’ SDOH needs with medically appropriate, cost-effective alternatives to traditional medical services.
- Value Added Benefits (VAB) — Medicaid health plans can offer VABs for food and nutrition programs without authorization from CMS.
- Public-private collaborations — One of the biggest opportunities for tackling SDOH and food insecurity is in expanding collaboration between public and private sector organizations. These public-private partnerships not only help merge payer resources but also scale programs and reach more underserved communities within each state.
Case studies
Around the nation, states are piloting programs to address food insecurity with positive results. Here are just a few examples:
California
Overview: Members in Medi-Cal (California’s Medicaid health care program) are being referred to the state’s Community Supports program which addresses SDOH including nutritional support. One successful pilot program was jointly run by Inland Empire Health Plan (IEHP) and Mom’s Meals. It included six months of medically tailored meals, fresh produce and nutrition education to certain dual eligible members with congestive heart failure and at least two recent hospital stays.
Outcome: The program resulted in a reduction in both trips to the emergency room and hospitalizations. Additional positive health outcomes included weight loss, greater medication adherence and significant cost savings. A reanalysis showed a lasting impact.
Georgia
Overview: Recent changes by the Georgia Department of Aging modernized nutritional requirements to allow person-centered nutrition and medically tailored meals to be included in state support programs.
Outcome: AAAs can now improve choice and access to nutrition programs and diversify providers to help reduce waiting lists, especially in high-risk areas.
Updated white paper offers ways to break down barriers to innovation

Innovating to Overcome Food Insecurity: How states are taking new approaches to achieve better outcomes shows you how programs can accommodate current day challenges — yet innovate — when addressing community-based hunger with:
- Government and state challenges and opportunities
- Case studies of state-level success
- 5 questions to answer to get successfully started

.jpg)
