Managed care organizations (MCOs) have traditionally focused on providing medical benefits such as doctor’s visits, hospitalizations, and prescription medications to care for members facing illness or injury. But as research grows on how upstream drivers of health (UDOH), also known as social determinants of health, impact health and well-being, managed Medicaid plans, as well as states administering Medicaid programs, are looking for ways to implement innovative, new benefits to help their members proactively address members’ unmet health-related social needs (HRSN).
Now the Centers for Medicare & Medicaid Services (CMS) is supporting some of those efforts by state Medicaid programs. With CMS approval, ILOS allow plans to substitute services or settings covered in a state Medicaid plan because they are medically appropriate and cost-effective alternatives to traditional benefits.
State ILOS examples
New York now has a state-wide medically tailored meal (MTM) ILOS program for high-need individuals and is launching a recently approved 1115 demonstration that will address UDOH and advance health equity. Included in the program are a number of services to address HRSN, including MTM, as well as support for greater integration between primary care providers, community-based organizations and behavioral health specialists. HRSN will go live in late 2024.
Iowa is expanding its HRSN footprint in a groundbreaking ILOS approval for MCO members who are on a 1915(c) home and community-based services(HCBS) waiver waiting list and not currently receiving these services. The MCOs now have authority to provide many long-term services and supports waiver services including MTMs.
CMS approved a proposal by California’s Medicaid plan, called Medi-Cal, to use Community Supports (California’s nomenclature for the proposed list of state-approved ILOS) to offer a set of 14 health-related, non-medical services to members. California is a vanguard when it comes to ILOS, but awareness and interest in the option is growing.
14 approved Community Supports in California
- Medically Tailored Meals
- Housing Transition Navigation Services
- Housing Deposits
- Housing Tenancy and Sustaining Services
- Short-Term Post-Hospitalization Housing
- Recuperative Care (Medical Respite)
- Day Habilitation Programs
- Caregiver Respite Services
- Nursing Facility Transition/Diversion to Assisted Living Facility
- Community Transition Services/Nursing Facility Transition to a Home
- Personal Care and Homemaker Services
- Environmental Accessibility Adaptations (Home Modifications)
- Asthma Remediation
- Sobering Centers
ILOS benefit to members
Members benefit from ILOS because they can have access to helpful services that address needs and improve health, such as condition-specific nutritious home-delivered meals, asthma remediation and home modifications. Under CMS rules, health plans can offer innovative services that help meet a person’s unique needs, particularly related to UDOH and health equity concerns.
ILOS benefit to health plans
CMS’ support of approved ILOS benefits is good news for managed care plans too. This benefit flexibility allows plans to focus on preventive solutions to keep members healthy and out of the hospital, which could improve outcomes and reduce costs. ILOS expenditures qualify as covered services for rate-setting, meaning their claims count toward the capitation rate. In addition, when ILOS are used to reduce waiting lists for other waivers, such as HCBS waivers, health plans not only can address the needs of members in a timelier manner, but they can also improve health outcomes and quality of life for members while reducing Medicaid spend.
How does it work?
There is no set list of ILOS benefits states can offer. Rather, it’s up to a state to seek CMS approval for services it proposes that are medically appropriate and cost-effective substitutes for Medicaid services. CMS approved a range of ILOS in California including nutritious meals, caregiver respite, home modifications, sobering centers, and more.
California pilot program
In June 2021, 93 dually eligible members from a Medicaid Plan in California with congestive heart failure, with a minimum of four emergency department visits in the last 12 months and a high-risk profile, took part in a six-month pilot program of receiving lower-sodium MTMs from Mom's Meals®. Participants also received other supports, including calls with registered dietitians, community health workers, and nurse case managers, as well as produce and pantry boxes to help them transition to healthy lifestyle habits.
Pilot results included:
- 42% reduction in inpatient acute admissions
- 39% reduction in inpatient length of stay
- 39% reduction in unavoidable hospitalization
- 40% reduction in emergency department conversions to inpatient
Significant decreases in self-reported swelling of hands, legs, and feet occurred between baseline and mid-program and between baseline to the end-of-program (p. <.0001). Although there were no significant changes between mid-program and end-of program, the self-reported reductions in swelling that occurred early in the program were sustained.
The pilot program was not without limitations, including but not limited to overlaps in the delivery of tailored meals and produce and pantry boxes, the small sample size, and other concurrent interventions, all of which limits the ability to generalize study findings to a larger population.
Mom’s Meals – your ILOS partner
Mom’s Meals provides the most comprehensive food as medicine solutions nationwide, including medically tailored meals. We’re setting the standard in the food as medicine space with real-world results that show fewer hospitalizations, better A1C control, stronger medication adherence and meaningful reductions in the total cost of care. From caregivers and case managers to payers and state and federal agencies, we’re the provider trusted to deliver scalable, evidence-based interventions for Medicaid, Medicare, long-term care and self-pay populations.
Rely on our expertise in partnering with managed care organizations and State Departments of Health in California, New York and other states to help inform your program.
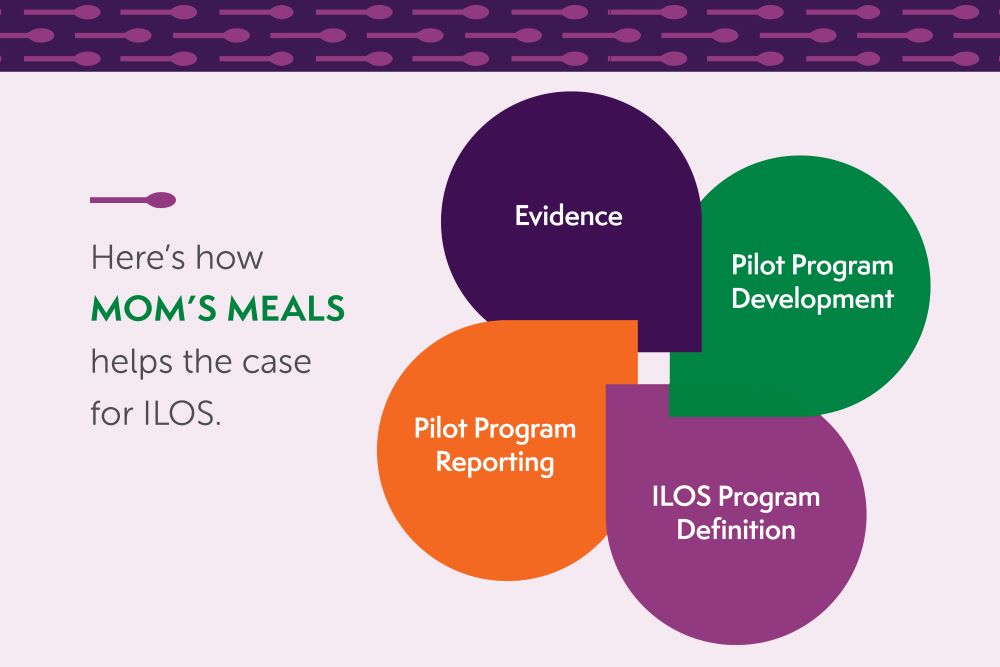
How Mom’s Meals helps
Evidence
- Laying groundwork for an ILOS program that includes medically tailored meals
Pilot Program Reporting
- Preparing data for internal and external stakeholders including state Medicaid directors and state departments of health
Pilot Program Development
- Identifying targeted members
- Developing protocols
- Measuring outcomes
ILOS Program Definition
- Eligible populations
- Credentialing
- Billing requirements
Considering ILOS for your plan but need support?
The Mom’s Meals team can help. Contact John Phillips, vice president, national program development at john.phillips@momsmeals.com or 888-343-8020.
Mom’s Meals food as medicine solutions
We provide nutrition solutions designed for all ages to bring comfort and inspire confidence in people seeking to live healthier, manage chronic conditions, recover from illness or continue to live independently. Our integrated solutions include medically tailored meals, produce and pantry boxes, oral nutrition supplements, shelf-stable, kosher and halal meals, and nutrition counseling and education.
Learn more about Mom's Meals food as medicine solutions.
.jpg)


