Countless studies prove the value of eating a healthy, balanced diet for everyone. But how does nutrition impact the chronically ill in terms of their health and health care bills? With six in ten U.S. adults living with a chronic illness, researchers are busy looking for answers.
A few of the most common — and costly — chronic illnesses in America are:
- Cardiovascular disease, including high blood pressure and high cholesterol
- Chronic lung disease
- Diabetes
- Kidney disease
Those diseases along with cancer, stroke and Alzheimer’s disease, are the leading drivers of our country’s stunning $4.5 trillion annual health care costs.
Each of those conditions can be prevented, managed and even treated in some cases with the right diet. However, the chronically ill often don’t have access to the foods they need due to social drivers of health (SDOH) including food and nutrition insecurity, transportation issues and living in food deserts or food swamps.
Research provides insight and answers
Finding ways to overcome those issues and support regular access to nutritious food for the chronically ill is critical. The results of these three studies demonstrate that making one important change — improving access to nutrition — has multiple benefits.
Study 1: Improving utilization and costs
Dietary factors are thought to contribute to hospitalization for patients with heart failure, but researchers wanted to learn more. A pilot study by Inland Empire Health Plan (IEHP) in California validates that theory.
Partnering with Mom’s Meals®, IEHP provided more than 28,000 medically tailored meals to dually eligible members who had congestive heart failure and a minimum of two hospital stays within the previous year. The program offered participants fully prepared lower-sodium meals, fresh produce and dry goods, plus nutrition education, a digital scale and home visits.
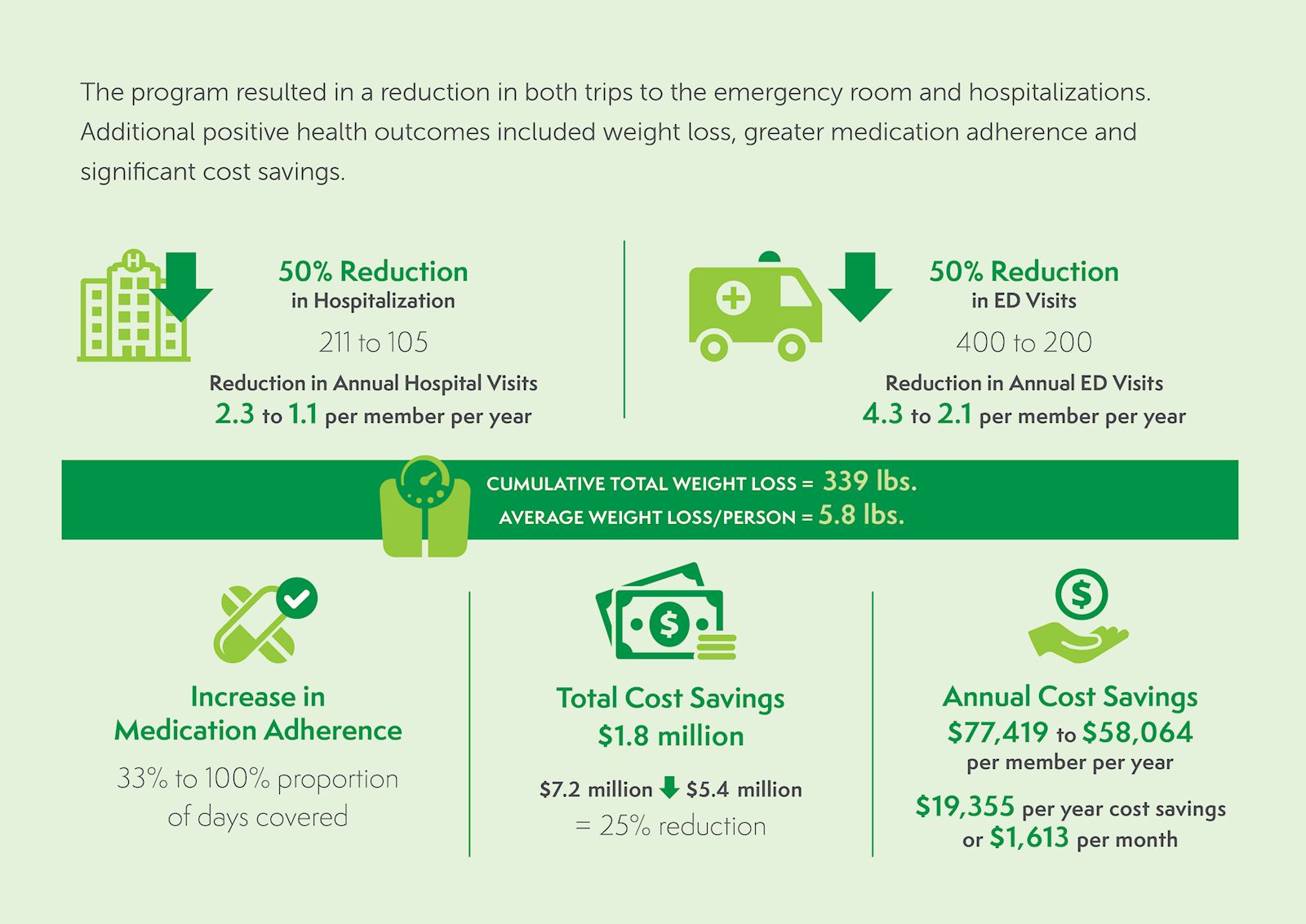
*This was primarily from decreased hospitalizations and associated costs.
Reanalysis shows lasting impact
Data for 93 enrolled members was reanalyzed 6 months after first analysis; 12 months after program end date and found:
- 42% reduction in hospitalizations
- 39% reduction in length of stay
- 21% reduction in total cost of care
Members also self reported:
- Improved access to healthy foods and lower salt consumption
- Reduced HF symptoms such as shortness of breath and swelling
Study 2: Lower readmission and address malnutrition
Many factors affect how someone recovers after a hospitalization, but experts agree that nutrition is one of the most important factors, especially for patients who have complex medical conditions.
Unfortunately, many people are at a nutritional deficit when they arrive at the hospital. Studies show that up to half of patients, especially older adults, admitted to the hospital are either at risk for malnutrition or are malnourished. And that makes them more likely to be readmitted.
A study by Kaiser Permanente of Southern California (KPSC) demonstrates that home-delivered meals provided to recently discharged patients help reduce rates of readmission and death post discharge.
During the study KPSC offered four weeks of Mom’s Meals home-delivered meals to an ethnically diverse cohort of almost 12,000 Medicare Advantage patients who were recently discharged from 15 Kaiser Permanente hospitals.
The study group’s outcomes were compared with two control groups, one from a 2019 historical study and another concurrent cohort that did not receive a meals benefit. Compared to the two control groups, the “meals benefit group” had lower odds of rehospitalization and death.
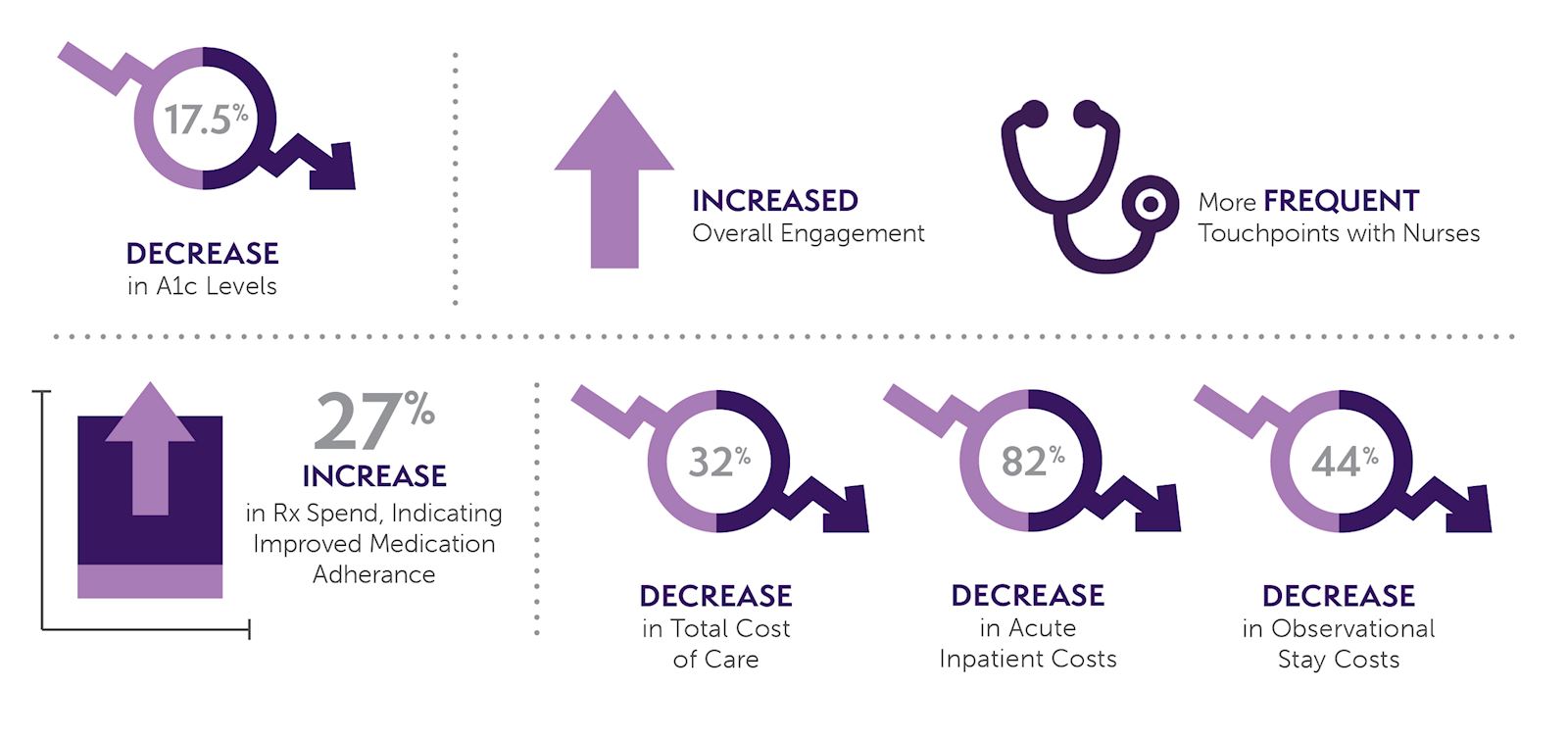
Study 3: Lower costs and address SDOH
Decades of research links food insecurity with poor health outcomes and shows clear disparities in diet quality exist due to social drivers of health (SDOH). It has an economic impact as well. Food insecure families spend 20% more in total health care expenditures compared to food secure families.
A pilot program by Health Plan of Nevada demonstrated how to increase food and nutrition security while decreasing total cost of care. The company partnered with Mom’s Meals to provide two home-delivered meals every day for eight weeks to enrollees who needed support with diabetes management. Participants also received disease management support and weekly contact with a registered nurse for 12 weeks.
The results were positive:
As research on improving access to nutrition continues to accumulate, it’s clear that nutritious, condition-appropriate meals can help patients — chronically ill, recently discharged and those facing food and nutrition insecurity — stay healthier. That can ultimately lower costs for the health care system and patients, while reducing mortality rates and supporting a higher quality, longer life for patients.
Mom's Meals can help
Mom’s Meals provides the most comprehensive food as medicine solutions nationwide. Together with health care and community partners, we empower people to live healthier lives through delicious, nutritious food, education, caring support and expertise.
Our nutrition solutions are designed for all ages to bring comfort and inspire confidence in people seeking to promote healthy living, manage or avoid chronic conditions, recover from illness, continue to live independently or simply enjoy convenient, trusted meals and support that fits their lifestyle. Our integrated solutions include medically tailored meals, produce and pantry boxes, oral nutrition supplements and shelf-stable, kosher, and halal meals, backed by nutrition education and counseling.


