More and more, hospitals and health systems are addressing the root causes of disease in their communities. That’s being driven by better research and more regulation.
In 2002, the Affordable Care Act (ACA) began penalizing hospitals with high readmission rates. For example, hospitals face up to a 3% cut in Medicare payments for having higher readmission rates for certain measures. Failing to lower patient readmission rates not only leads to strong financial penalties, but also to fewer — or potentially lost — referrals and higher costs to deliver care.
One thing most organizations are focusing on to reduce hospital readmissions is nutrition. It’s part of the wider food as medicine movement that recognizes that diet has the potential to cause disease, as well as the potential to prevent, reduce and even reverse some conditions. As a result, quality nutrition can help improve the total cost of care.
That’s why prevention and post-discharge nutrition-based resources, programs and incentives are now central to many health plans including Medicare Advantage plans. They’re needed more than ever as food insecurity and chronic conditions are on the rise in America:
- 34 million Americans are food insecure
- 1 in 14 seniors were food insecure in 2021
- In the past two decades, food insecurity has increased by 45% among older adults
- 60% of older adults have at least two chronic conditions
The nutrition-readmission connection
How does nutrition connect with hospital admissions? Studies show that good nutrition is foundational to the healing process after a hospital stay because it promotes recovery and independence, and better health helps reduce readmissions.
- As many as half of patients admitted to the hospital are at risk for malnutrition or are malnourished, particularly older adults.
- A study published by Avalere Health in partnership with the Academy of Nutrition and Dietetics and other stakeholders, showed that malnourished adult inpatients have a 54% higher likelihood of 30-day hospital readmissions than patients who are well-nourished.
- The average cost per readmission were 26-34% higher for patients with malnutrition compared to those without malnutrition.
One solution: Home-delivered meals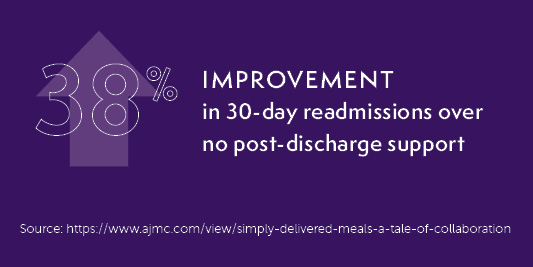
Post-discharge meals have proven to be a big deterrent to hospital readmissions, since post-discharge meals help ensure patients continue to receive proper nutrition once they leave the hospital.
This is especially key for patients suffering from a chronic condition, which puts them at risk for malnutrition. Patients with chronic conditions like diabetes or heart disease may require a diet low in sugar, fat, sodium or cholesterol. Post-discharge meals are equally important to individuals who simply cannot prepare meals for themselves or whose caretakers don’t know how to fulfill their nutritional needs, as well as those who are food insecure.
Case in point: Kaiser Permanente Southern California (KPSC)
A new study reported in JAMA Health Forum reinforces the importance of convenient access to good nutrition as one of the most important factors in successful post-discharge healing. For the research, KPSC offered four weeks of Mom’s Meals® home-delivered meals to an ethnically diverse cohort of almost 12,000 Medicare Advantage patients who were recently discharged from 15 Kaiser Permanente hospitals. Study participants had been admitted to the hospital for heart failure or other acute medical conditions.
Results from the study group, or “meals benefit” group, were compared with two control groups, one from a 2019 historical study and another concurrent cohort that did not receive a meals benefit. The KPSC study showed patients who received the Mom’s Meals home-delivered meals benefit had lower odds of 30-day rehospitalization and death, and providing convenient access to quality nutrition through home-delivered meals may improve outcomes for older adults.
Mom's Meals®
New white paper: The Power of Food as Medicine: What Health Care is Doing and What is Working
There is still much work to be done to bridge the continuum of care from hospital to home or living facility. One thing is for certain: by using food as medicine, we can drive change. Our new white paper proves how together — through quality nutrition — health plans, government entities, public and private organizations, and individuals can better integrate the food as medicine concept into services and benefits for better outcomes and lower health care costs for all.
Post-discharge care program
Mom’s Meals offers a post-discharge care program that provides expedited nutritional support to patients at the start of their recovery from a hospital or skilled nursing facility stay. We work with health insurers, health systems, hospitals and other health care organizations to create post-discharge meal delivery programs that work for their members and patients.