Categorizing a year in one word is difficult, but when it comes to health care, “change” is apt for 2023 and the forecast for 2024.
In 2023, the end of the COVID-19 public health emergency (PHE) spurred more changes in an already volatile health care industry. Many of those changes carry over to 2024 and include pressure for better results and access; new funding approaches, partnerships and care delivery methods; and modifications to Medicare and Medicaid policies.
A focus on food and nutrition
The pace of change in health care will only accelerate in 2024. And the role of food and nutrition — in terms of access, outcomes, costs, benefits and more — will be a big focus largely because the federal government is creating greater momentum to end hunger and improve nutrition for Americans. In March 2023, The White House Challenge to End Hunger and Build Healthy Communities announced new actions to encourage public and private stakeholders in all sectors to do more to end hunger, increase healthy eating and physical activity for Americans by 2030.
The administration’s focus on food and nutrition is spurring more collaboration and partnerships focused on research and pilot programs. What could that look like?
- Pilot tests of medically tailored meals (MTM) for Medicare fee-for-service members
- States testing Section 1115 Demonstration waivers for MTMs for Medicaid members
- More programs to increase access to food and nutrition for vulnerable populations
How Medicare Advantage (MA) and Medicaid are changing to emphasize food and nutrition.
Medicare Advantage
MA plans to continue to grow. A recent KFF study shows that between 2022 and 2023, MA enrollment grew by 8%. Now, just over half, or 51%, of all Medicare-eligible people in the U.S. are covered by an MA plan.
In tandem with that growth, Centers for Medicare & Medicaid Services (CMS) are making changes to ensure that MA plans are effectively addressing social determinants of health (SDOH) and health equity.
Rates and stars changes
CMS is implementing major updates to drive more equitable, high-quality, affordable care. The 2024 rate increase of 3.32% is smaller than the past several years. CMS also revised the star ratings calculation to emphasize member experience and health equity. That resulted in many plans receiving lower star ratings and, therefore, fewer rebate dollars.
Those changes mean MA plans need to do more with less to provide the most value to members. To do that, plan designers are focusing on high-impact benefits like nutrition programs and home-delivered meals programs (HDM) that provide the most value to members and help keep them engaged.
Example
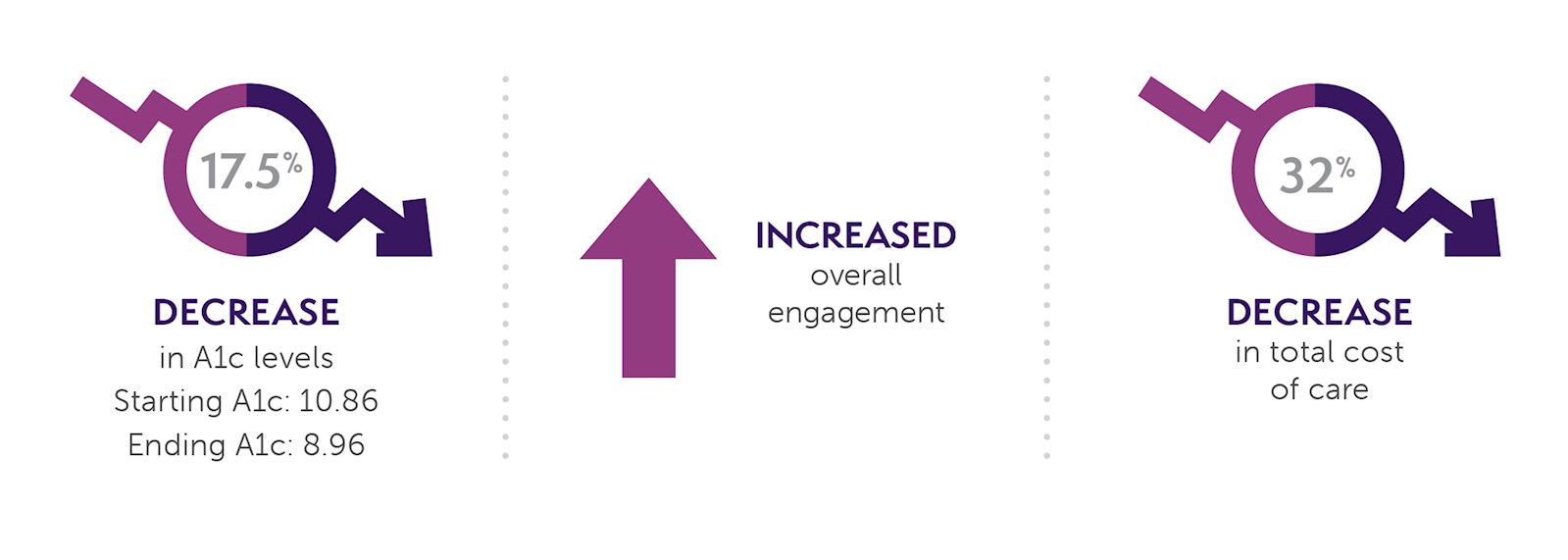
Heath Plan of Nevada, a UnitedHealthcare® Company, partnered with Mom’s Meals® to create a pilot program to support diabetes management, by better engaging its members as well as addressing food insecurity and SDOH. The pilot program launched in September 2020 with results including:
Draft rule has an impact
While it’s not final, the CMS draft final rule is already influencing how MA plans design benefits to address new requirements about accessing benefits and using evidence-based solutions. Starting in 2025 MA plans may be required to send mid-year notifications to each member about their available and unused benefits. Also, Special Supplemental Benefits for the Chronically Ill (SSBCI) must be evidence-based and include a bibliography.
MTMs are backed by 20 years of research proving their efficacy, making them a valuable — and popular — benefit for MA plans to offer. Mom’s Meals is proud to have been involved in five peer-reviewed published MTM studies and can support the need for a bibliography or evidence.
Spotlight: Research shows HDMs improve outcomes
JAMA Health Forum published an analysis of impact of post-discharge meals in MA members. In the Kaiser Permanente Southern California study, four weeks of Mom’s Meals HDMs were offered to an ethnically diverse cohort of almost 12,000 MA patients who were recently discharged from 15 Kaiser Permanente hospitals for heart failure or another acute medical condition.
Compared to two control groups, patients in the study group or “meals benefit” group, had lower odds of 30-day rehospitalization and death. In short, providing convenient access to quality nutrition through HDMs may improve outcomes for older adults.
Medicaid
With food insecurity for all populations at all-time highs, CMS is providing more guidance and pathways to help states and managed care plans address SDOH and health-related social needs (HRSN). In 2023, more Medicaid plans used 1115 demonstrations and In Lieu Of Services (ILOS) programs to address food and nutrition-related needs. That’s expected to continue in 2024.
Addressing SDOH via ILOS
CMS guidance encourages states and managed Medicaid health plans to use ILOS programs to include MTMs in their Medicaid programs. States can pay for preventative services, such as HDMs, in lieu of more expensive, downstream services such as hospitalizations. In addition, states are working to address home and community-based services waiting lists with care plans and ILOS with greater recognition of the many barriers those on the waiting lists are facing.
The CMS November 2023 HRSN bulletin provides new guidance for addressing HRSN to improve access to care and outcomes for Medicaid enrollees. It includes flexibility in how states select providers and which services they offer. The bulletin lists 15 CMS-approved HRSN services for Medicaid including food and nutrition services.
The government, health plans and providers are all working on improving health equity to ensure better access to services and benefits for all groups defined by race/ethnicity, sexual orientation, age, gender identity, disability status and income.
AARPs LTSS 2023 State Scorecard Report is a useful tool comparing state long-term services and supports (LTSS) systems. Reflecting the national focus on equity, this year’s report uses updated calculations for scoring states including 11 indicators using race/ethnicity data.
Improving maternal mortality rates is a major health equity focus as the U.S. is in a maternal health crisis. To address differences in maternal mortality across racial and ethnic groups, managed care plans and states are introducing new benefits like doula services to pregnant people and increasing post-partum coverage.
Improving HCBS waiver program outcomes
States are recognizing historical limitations with current home and community-based services (HCBS) waivers that limit the ability to improve food security outcomes. There is not only rising advocacy to ensure meal benefits address rising food insecurity rates within this population, but to also support national goals around LTSS rebalancing, person-centered care planning, and the promotion of general health and well-being.
As CMS continues to update guidelines on modernizing person-centered outcomes within the HCBS population, any language reducing the ability for food insecure individuals to qualify for HDMs can be updated to promote consistent access and consumption of healthy food.
Evaluating IDD waiver program guidelines
Momentum around the addition of HDM benefits to intellectual and developmental disabilities (IDD) waiver programs continues to grow. As states look at modernizing the guidelines of these programs, the addition of medically tailored HDMs to IDD waivers can help improve outcomes around health condition management and food security rates, along with the promotion of independence and dignity, and alignment around person-centered care planning.
Spotlight: Redetermination spurs innovative communication
When the COVID-19 PHE ended, so did the continuous Medicaid enrollment process that kept millions of Americans protected with health care coverage during the pandemic. According to the KFF, by January 9, 2024, more than 14 million Americans had been disenrolled due to the change called “redetermination.” The process required managed Medicaid plans to get creative about notifying members about their eligibility. Mom’s Meals played a critical role for MCOs who used Mom’s Meals meal cooler inserts, conversations with their Mom’s Meals delivery drivers and outbound calls from the Mom’s Meals customer service center to reach their members.
Helpful resources
As we head into 2024, health plans, state Medicaid leaders, case managers and community programs will see how continuing changes in health care and the emphasis on food and nutrition shape their work. Keep these helpful resources on hand:

Discover how to improve your plan’s star ratings by incorporating medically tailored, home-delivered meals benefits with our Guide for Medicare Advantage Plan Product and Clinical Teams: Improving Outcomes and Star Ratings Through Food and Nutrition Benefits Design.

Innovating to Overcome Food Insecurity: How states are taking new approaches to achieve better outcomes shows you how programs can accommodate current day challenges — yet innovate — when addressing community-based hunger with:
- Government and state challenges and opportunities
- Case studies of state-level success
- 5 questions to answer to get successfully started